Getting your blood tests done is a very important part of your fertility journey. Your blood holds important clues about your health, your body’s function, and also your fertility. Here at NSA, we go beyond the conventional “normal” ranges provided by mainstream medicine. There is an important difference between blood test result that are in the “normal range”, versus results that are in the “optimal range” for fertility. So we interpret your test results through the lens of optimal health, especially for those on the path to parenthood. In this blog, we look at a few key blood tests to pay close attention to.
Key Blood Test 1: Iron
 Iron is often overlooked but it plays an important role, particularly in fertility and pregnancy. For women, iron deficiency is commonly due to monthly blood loss during menstruation. During pregnancy, the demand for iron skyrockets to support the growing foetus and the expansion of the mother’s blood volume.
Iron is often overlooked but it plays an important role, particularly in fertility and pregnancy. For women, iron deficiency is commonly due to monthly blood loss during menstruation. During pregnancy, the demand for iron skyrockets to support the growing foetus and the expansion of the mother’s blood volume.
When iron levels are low, your body prioritises supplying blood to essential organs like the brain and heart. This leaves the blood supply to reproductive organs at the bottom of the list which could cause problems with fertility.
In our clinic, we frequently encounter patients with low ferritin levels (ferritin is the stored iron). This may require an iron supplement or even an iron infusion. It is however important to note that ferritin levels can rise in response to inflammation or infection. Therefore, by merely testing ferritin levels we may overlook iron deficiency.
It is always important to get a comprehensive iron study done. This includes an iron and transferrin level, the iron saturation, and a ferritin level. This is essential for a thorough understanding of your iron status and your fertility.
Key Blood Test 2: Vitamin D
Vitamin D is often recognised as an immunity booster but it also plays an important role in fertility. It is involved in hormonal regulation and it influences the production of oestrogen and testosterone. These hormones are essential for the development of eggs and sperm.
A 2017 study revealed that women with lower levels of vitamin D may face challenge in conceiving [1]. Furthermore, research has provided reassuring evidence regarding the safety of vitamin D supplementation during pregnancy. A study done in 2011 demonstrated the safety and effectiveness of pregnant women taking up to 4000iu of vitamin D during pregnancy [2].
Even though western medicine regards a level of 50 nmol/l or above sufficient, a level of around 100 nmol/l is a more optimal level for fertility from our point of view.
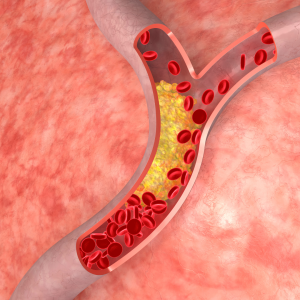 Key Blood Test 3: Cholesterol
Key Blood Test 3: Cholesterol
While high cholesterol levels can disrupt hormonal balance and affect fertility, having excessively low cholesterol levels can also pose risk.
Cholesterol serves as the building blocks for sex hormones such as oestrogen, progesterone, and testosterone. Maintaining an optimal cholesterol level is crucial for hormonal balance and reproductive health.
Do you need help with interpreting your Blood Test results?
Are you trying to conceive and seeking more insight into your fertility journey? Here at Natural Solutions Acupuncture our practitioners have the ability to analyse fertility from the perspective of both Western and Chinese Medicine. This offers a comprehensive and integrative approach to crafting the best treatment plan for you to optimise your fertility. You can book your appointment online here.
References:
[1] Fung, J.L. et al. (2017) ‘Association of Vitamin D intake and serum levels with fertility: Results from the lifestyle and fertility study’, Fertility and Sterility, 108(2), pp. 302–311. doi:10.1016/j.fertnstert.2017.05.037.
[2] Hollis BW, Johnson D, Hulsey TC, Ebeling M, Wagner CL. Vitamin D supplementation during pregnancy: double-blind, randomized clinical trial of safety and effectiveness. J Bone Miner Res. 2011 Oct;26(10):2341-57. doi: 10.1002/jbmr.463. Erratum in: J Bone Miner Res. 2011 Dec; 26(12):3001. PMID: 21706518; PMCID: PMC3183324.

